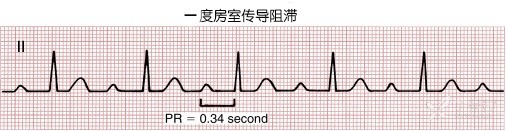
First-degree atrioventricular block
OVERVIEW
What is first-degree atrioventricular block?
First-degree atrioventricular block occurs when the impulse from the atria is conducted through the atrioventricular node, with conduction ultimately completed but delayed compared to the normal conduction time. The corresponding electrocardiogram change shows a prolonged PR interval (greater than 0.20 seconds), representing delayed atrioventricular conduction.
Are there other types of conduction blocks besides first-degree atrioventricular block?
Yes, other types include second-degree atrioventricular block, third-degree atrioventricular block, right bundle branch block, and left bundle branch block.
SYMPTOMS
What are the manifestations of first-degree atrioventricular block?
Generally, there are no symptoms. Patients with organic heart damage may exhibit corresponding manifestations. The electrocardiogram shows uniformly prolonged PR intervals, which are fixed but consistently exceed 200ms. (See image below)
The block site in first-degree atrioventricular block is entirely within the His-Purkinje system. His bundle electrograms confirm that the block occurs in the mid or lower segment of the His bundle in 35% of cases and in the upper segment in 65%. Chen Xin et al. (1997) noted no reports of blocks occurring in the atrioventricular node or atria. On surface electrocardiograms, approximately 29% of patients exhibit narrow QRS waves (≤ 0.10 s), while about 71% show wide QRS waves (≥ 0.12 s).
CAUSES
How does first-degree atrioventricular block occur?
First-degree atrioventricular block may occur in:
-
Healthy individuals with high vagal tone;
-
Conditions such as myocardial ischemia, myocardial infarction, acute rheumatic fever, myocarditis, or cardiac degenerative changes;
-
Medications like digoxin, calcium channel blockers, or beta-blockers;
-
Congenital heart diseases: atrial septal defect or patent ductus arteriosus.
What does atrioventricular block mean?
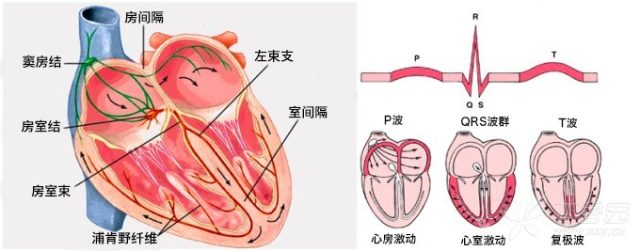
Atrioventricular block refers to abnormal impulse conduction between the atria and ventricles. It may involve complete blockage, partial blockage, or delayed conduction. The blockage can occur in the atrioventricular node, His bundle, or bundle branches.
What is normal atrioventricular conduction?
The cardiac conduction system consists of specialized myocardial cells that generate and transmit impulses, including the sinoatrial node, internodal tracts, atrioventricular node, atrioventricular bundle (His bundle), right bundle branch, and Purkinje fibers. The sinoatrial node is the natural pacemaker of the heart. The internodal tracts conduct impulses between the sinoatrial and atrioventricular nodes. The atrioventricular node and bundle form the atrioventricular junction, extending downward to the membranous septum, where it divides into left and right bundle branches beneath the endocardium. The left bundle branch further splits into anterior and posterior fascicles, while the right bundle branch descends along the right side of the septum, branching into Purkinje fibers near the apex. These fibers connect with ventricular muscle, coordinating rhythmic contractions of the atria and ventricles. The cardiac conduction system is illustrated below:
Does first-degree atrioventricular block affect specific populations?
No. Clinically, this type of arrhythmia does not require special management or labeling—it is merely an incidental finding.
DIAGNOSIS
What are the ECG manifestations of first-degree atrioventricular block?
Typical ECG characteristics of first-degree atrioventricular block:
-
Every sinus P wave can conduct to the ventricles and produce a QRS-T complex.
-
P-R interval > 0.20 s (in adults); P-R interval ≥ 0.18 s in children (under 14 years old).
-
P-R interval exceeds the normal upper limit (depending on heart rate).
-
When there is no significant change in heart rate, an increase in P-R interval by more than 0.04 s compared to previous measurements can still support the diagnosis, even if the P-R interval remains within the normal range.
TREATMENT
How to treat first-degree atrioventricular block?
Generally no treatment is needed. Patients with organic heart disease should manage the primary condition. Prognosis is unrelated to whether the first-degree AV block is corrected.
Can first-degree atrioventricular block fully recover after treatment?
Prognosis depends on whether there is underlying organic heart disease. If not, there is no need for concern. If present, simply managing the existing heart condition is sufficient.
What to do with first-degree AV block accompanied by right bundle branch block?
The right bundle branch is naturally prone to block due to its slender structure, which is clinically common and requires no special treatment. The combination of both conditions is not a cause for concern—just ensure heart rate and blood pressure remain controlled. If sudden ECG changes occur, consider signs of increased right heart load and actively investigate potential causes, remaining vigilant for pulmonary embolism.
DIET & LIFESTYLE
What impact does first-degree atrioventricular block have on normal life and work?
Generally, there are no symptoms. However, for patients with tachyarrhythmia, when using medications to slow the heart rate, it is important not to reduce the heart rate below 60 beats per minute to avoid potential risks. Regular monitoring is sufficient.
What should patients with first-degree atrioventricular block pay attention to in terms of diet and lifestyle?
Patients with heart disease are more prone to developing heart block. Adopting heart-healthy measures can help prevent heart disease:
-
Healthy diet: Eat more fruits, vegetables, and low-fat dairy products, and reduce intake of meat or fatty foods.
-
Engage in regular walking or physical activity.
-
Lose weight if overweight.
PREVENTION
How to effectively avoid first-degree atrioventricular block?
Clinically, there are almost no definite complaints of discomfort. It is often discovered incidentally during electrocardiogram examinations and may be found in routine physical check-ups of healthy individuals, making it impossible to effectively prevent. If it coexists with organic heart disease, no separate treatment is required.